Does Worship Singing Spread Coronavirus?

For most Christians, communal singing—or singing with others in the congregation—is an important part of a worship service.
Recognizing this, many churches have tried to include hymns or worship songs in their online services. As these churches transition back to in-person services, however, they are reluctant to include congregational singing in those services.
The reason is simple: congregational singing spreads coronavirus.
Or does it? And, if so, how much?
March: Outbreaks in Choirs
Several high-profile coronavirus outbreaks occurred at choir practices and performances in March.
After a rehearsal on February 25, the 130-member Amsterdam Mixed Choir recorded the first official COVID-19 infection in The Netherlands. At the March 3 rehearsal, several sick members sat out. A March 7 dress rehearsal for a concert saw 15 singers sick, with many hoping to feel better in time for the concert. That concert, a performance of Bach’s St. John’s Passion for an audience of 1,000 in the Concertgebouw, went well, but 30 members sat out. In the ensuing month, 102 choir members contracted COVID-19. One died, as did three partners of choir members.
In Germany, five days after the March 9 rehearsal of the Berlin Cathedral Choir, one of the ensemble's 80 singers contacted the choir director to say that she had tested positive for COVID-19. Within two weeks, about 30 members had tested positive, and another 30, plus the director, were showing symptoms.
On March 10, half of the 122 members of the Skagit Valley Chorale attended a two-and-a-half hour choir practice at a Presbyterian church building in Mount Vernon, Washington. A greeter offered hand sanitizer at the door. Singers refrained from the usual hugs and handshakes, but according to a CDC report, they sat close to each other during the rehearsal, which was held in a room roughly the size of a volleyball court. Some shared snacks, such as mandarin oranges, and others stacked chairs at the end of practice. Unbeknownst to anyone, one person at the practice was infected and symptomatic. Of those who attended practice, 53 became infected (33 confirmed and 20 probable). Three were hospitalized, and two died.
No one is sure how much of the coronavirus spread at these choir practices was due to infected choir members singing. Would social distancing, or having the singers at least six feet apart, have helped slow or even stifle the spread? That depends on how the virus is spread.
How Coronavirus Spreads
After several months of intensive research worldwide, scientists are beginning to understand how the so-called “novel coronavirus” (2019-nCoV, or SARS-COV-2) and the disease that it causes (COVID-19) spread. That spread is greatest where there is close contact and crowding in closed spaces, says Muge Cevik, a virologist at the University of St. Andrews in the United Kingdom, who has been collecting and reviewing research papers, primarily from China, Singapore, and Taiwan.
The average infected individual transmits the virus to between two and three others. But that’s an average. In the real world, most infected people transmit the disease to one or no others, while a minority infect many others in so-called super-spreading events. In fact, 9 percent of infected people are responsible for 80 percent of the transmissions.
According to Cevik, the disease apparently is very infectious only for a short window, and perhaps only in some cases. Infected people are most infectious right around the onset of symptoms, as well as a couple of days before and after. If someone in that stage spends concentrated time with others in a confined space, many of those people probably will get sick.
Length of exposure matters as much as distance from other people. People passing by you in a supermarket are unlikely to infect you. Outdoor environments appear much safer as well. In one study, which followed hundreds of cases, all but one transmission occurred indoors.
Guidance on the Centers for Disease Control (CDC) website reflects these research findings. “COVID-19 is thought to spread mainly through close contact from person-to-person,” it says. Transmission is believed to be when “respiratory droplets produced when an infected person coughs, sneezes, or talks…land in the mouths or noses of people who are nearby or possibly [are] inhaled into the lungs.”
The modifier “possibly” reflects on ongoing debate about whether or not coronavirus is transmitted through the air and inhaled.

The Potential Role of Aerosols
A person who is infected with a respiratory virus expels two types of droplets that may contain the virus. Larger droplets, called respiratory droplets, are greater than five micrometers (5 μm) in diameter and are not thought to be inhaled by others. Smaller droplets (less than 5 μm), called droplet nuclei or aerosols, travel further, stay airborne longer, and can be inhaled by others.
According to the World Health Organization (WHO) website, coronavirus transmission through respiratory droplets occurs when:
- A healthy person is within a few feet of an infected person
- The infected person emits infective respiratory droplets
- Those droplets enter the mouth, nose, or eyes of the healthy person
Can someone get coronavirus via airborne transmission, or by inhaling aerosols from an infected person? The WHO maintains that, outside of a few hospital procedures (such as endotracheal intubation, bronchoscopy, and open suctioning), coronavirus is not transmitted through aerosols. In an analysis of 75,465 COVID-19 cases in China, no airborne transmission was reported.
Dr. Benedetta Allegranzi, WHO technical lead of infection prevention and control, wrote in a May 31 email that, despite theories based on lab simulations, “there is no evidence of transmission of the virus as an airborne pathogen.” A group of experts that reviews evidence with WHO weekly has “not judged the existing evidence sufficiently convincing to consider airborne transmission as having an important role in COVID-19 spread.”
Lidia Morawska, an aerosol researcher in Australia, disagrees. She says that WHO’s conclusions stem from a belief that aerosols travel only an arm’s length in the air. The CDC report on the Skagit Valley Chorale states that the “act of singing, itself, might have contributed to transmission through emission of aerosols, which is affected by loudness of vocalization.”
A Lack of Research on Singing
The CDC report refers to a 2019 scientific study that examined aerosol emissions not from singing but from talking. In addition to finding that the rate of aerosol emission is positively correlated with the loudness (amplitude) of vocalization, researchers found that a small fraction of individuals are “speech superemitters,” consistently releasing an order of magnitude more particles than their peers and potentially acting as disease superspreaders.
Does singing act like speech? Few studies have been done. A commonly cited one investigated the potential role of singing in spreading tuberculosis. That study found that singing produced 39% as many droplets as talking and 10% as many droplets as coughing. After 30 minutes, more singing droplets than talking droplets were still airborne (in a confined space, a box).
That study was conducted in 1968. Fortunately, the current pandemic has spurred more studies into singing and its role in spreading viruses.
In early May, two researchers at the Bundeswehr University in Munich published a paper entitled “Singing in choirs and making music with wind instruments ‒ Is that safe during the SARS-CoV-2 pandemic?” Their study showed that singing disturbs air flow only up to 1.6 feet in front of the person. The researchers even made a video to present their findings.
After conducting a similar study with similar results, Freiburg University's Institute for Performing Arts Medicine published guidelines for singing, including limiting the number of people in the room, limiting the length of rehearsals, staying two meters apart, keeping rooms ventilated, screening choir members, and wearing masks. Institute head Bernhard Richter gave one caveat: the researchers did not make any aerosol measurements.
"This is a work in progress," he said. "Of course singers want clear statements, black and white, but then you have to say, maybe we don't know yet."
Singing in Church: Germany vs. The U.S.
When Germany locked down in mid-March, religious services were banned. As restrictions began to ease in late April, Angela Merkel met with leaders of the country’s 16 states to coordinate a nationwide set of rules, including rules to govern worship services.
Communal singing proved to be a sticking point in the discussions, with leaders initially proposing a nationwide ban. “If the distance rules are abided by, there is no reason why singing should be refrained from altogether,” the German Bishops Conference said in its own position paper. A spokesman added, “We believe quiet singing and praying should be possible.”
In the end, the German federal government did not impose a nationwide ban but stated that singing should be avoided "because of the increased production of potentially infectious droplets, which can be spread over greater distances". Several German states have banned all singing from services.
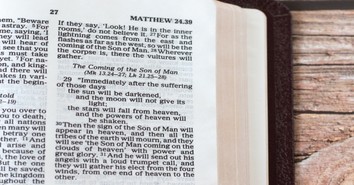
In the U.S., the CDC’s “Interim Guidance for Communities of Faith” initially included this recommendation: “Consider suspending or at least decreasing use of a choir/musical ensembles and congregant singing, chanting, or reciting during services or other programming, if appropriate within the faith tradition. The act of singing may contribute to transmission of COVID-19, possibly through emission of aerosols.”
That recommendation was removed on the current guidance page, as were recommendations on eliminating lines without six feet between attendees, encouraging the use of cloth face coverings, adding additional services, using video streaming or drive-in options for services and other gatherings, and having clergy hold virtual visits instead of in-home and in-hospital visits.
So, for now, the debate about the safety of worship singing will continue, in the U.S. and around the world.
Photo Credit: ©GettyImages/Prostock-Studio

Originally published June 11, 2020.